What Exactly is a Yeast Infection?

“Yeast infection” is the commonly used term for “Vaginal candidiasis”, “Candida vulvovaginitis”, “Vulvovaginal candidiasis” or just “VVC”. Despite the sound of its tongue-twisting names, the condition isn’t dangerous, but it can be extremely uncomfortable and occasionally challenging to get rid of.
If you have a vagina, chances are very high that you will develop at least one or more yeast infections – if you haven’t had one already.
What Exactly Is A Yeast Infection, Or “Vulvovaginal Candidiasis”?
Let’s break it down:
The vulva is the external genital area surrounding the vagina. It includes the clitoris, the inner and outer lips (labia) of the vagina, the opening to the urethra, the padded area called the mons pubis, and several smaller structures.
The vagina is the stretchy, lubricated tube that connects the external genitalia to the cervix.
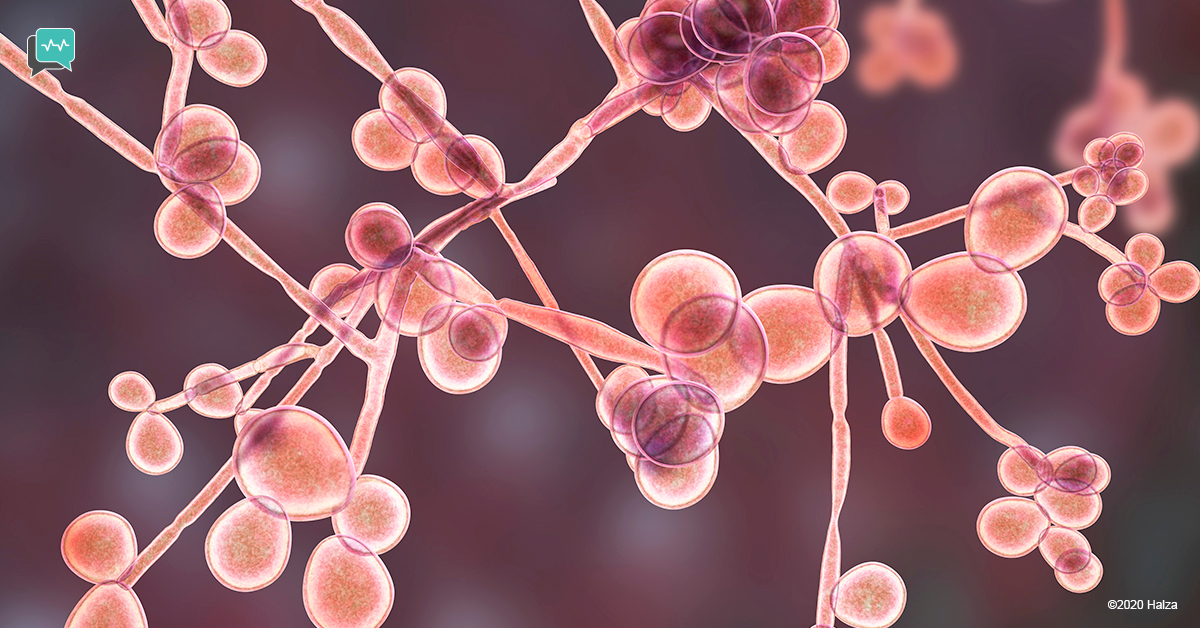
Candida is a yeast. Yeast is a type of fungus. Under ordinary conditions, Candida is simply part of the normal “flora” – the collection of various microorganisms that we all have in and on our bodies. Around 20-25% of females have candida in the vagina, where it peacefully coexists with other fungi and bacteria.
However, under certain conditions, Candida can grow out of proportion to the other microorganisms. As the Candida grows, it invades the surface cells of the vagina and vulva and causes the symptoms of a yeast infection.
The species of Candida that causes most yeast infections is “Candida albicans”.
What Are The Symptoms Of A Yeast Infection?
Symptoms vary from person to person, but can include:
- Intense itching (the most common symptom)
- Burning
- Soreness
- Irritation
- Pain during intercourse
- Vaginal discharge
– Often looks thick and white, like cottage cheese
– Can also be thinner and more watery - Minimal or no odor
- Pain while urinating
- Swelling
- Infection caused by scratching inflamed skin
Are Yeast Infections Sexually Transmitted Infections (STIs)?
Although Candida can be transmitted through sexual intercourse, yeast infections are not categorized as STIs.
Unlike STIs, yeast infections can develop in celibate women. And unlike the microorganisms that cause STIs, Candida can be part of the normal flora of both the vagina and the penis.
Candida overgrowth on the penis, called “candidal balanitis”, develops more often on uncircumcised penises than on circumcised ones.
Who Gets Yeast Infections? What Are the Risk Factors?

Candida thrives in the presence of estrogen. Therefore, people most likely to develop yeast infections are:
- People who are pre-menopausal (menstruating age)
- People who take supplemental estrogen.
- People who are pregnant.
Other risk factors for developing yeast infections include:
- High blood sugar from diabetes.
– Excess sugar is excreted in the urine. The sugar helps Candida adhere to the vaginal surface, preventing the immune system from keeping it in check.

- A weak immune system because of
– a medical condition
– medication that suppresses the immune system - Recent antibiotic use.
– Antibiotics can kill off ‘good’ bacteria that help to keep Candida in balance with other microorganisms. - Genetic predisposition.
– Gene mutations can prevent an immune response to Candida overgrowth or can cause hyper-reactions to Candida. - Oral contraception (“the Pill”). Oral contraceptives that increase estrogen levels can increase risk.
Related reading:
How Can I Prevent Yeast Infections from Developing?
There are no guaranteed ways to prevent yeast infections, but there are steps you can take to reduce your risk.
- If you have diabetes, follow your diet, exercise, medication, and testing recommendations to keep blood sugar levels within the target range.
- Don’t douche. Douching cleans out some of the bacteria that help to keep Candida at normal levels.
- Only use antibiotics when prescribed by your health care provider, and only use them if absolutely necessary. And always finish the full course, even if you feel better sooner.
- A dose of an oral antifungal medication called fluconazole at the start and end of antibiotic treatment might prevent a yeast infection from developing.
Several other factors are commonly thought to support Candida overgrowth, but scientific research is not definitive. If you are concerned about developing a yeast infection, it can’t hurt to take the following precautions:
- Change out of wet bathing suits after swimming.
- Wear underpants that have a cotton crotch.
- Change underpants after sweating.
- Wear underpants and pants that fit comfortably.
- Use only unscented products around the genital area.
Supplements advertised to help prevent Candida infections may or may not be effective, depending on the supplement and your specific circumstances. Consult your doctor before taking any supplements to prevent a yeast infection.
How Are Yeast Infections Diagnosed?
The symptoms of a yeast infection can overlap with several other vaginal infections. Therefore, anyone experiencing symptoms for the first time should see their health care provider. Self-diagnosis of yeast infections is inaccurate more often than accurate.
Conditions that have symptoms in common with yeast infections include:
- Trichomoniasis
- Chlamydia
- Gonorrhea
- Bacterial vaginosis,
- Vaginal atrophy
- Hypersensitivity reaction
- Contact dermatitis,
- Lichen planus
- Lichen sclerosis
- Allergic reaction
Over-the-counter treatments for yeast infections will not help the above conditions.

To determine if your symptoms are caused by a yeast infection, the health care provider will use a cotton swab to gently take a sample of the surface of the vagina. They will look at the sample under the microscope. If you have symptoms of a yeast infection but no yeast or other infectious organism is seen under the microscope, the provider will send the sample to a lab for culture.

Sometimes a pap smear result shows Candida even though you don’t have any symptoms. Since Candida can be part of normal flora and has no negative effects on the cervix, there is no need for treatment.
If you have had recurrent yeast infections that are not responding to treatment, your provider should send a sample out to a lab that can check for resistance to the type of treatment.
Related reading:
What Are the Treatments For Yeast Infections?
The treatment depends on whether the infection is “uncomplicated” or “complicated”. “Uncomplicated” refers to:
- three or fewer than 3 yeast infections per year
- mild to moderate symptoms
- a normally functioning immune system
- not pregnant; and
- the most likely diagnosis is Candida albicans.
Uncomplicated yeast infections are usually treated with a single 150mg dose of oral fluconazole or with one to three nightly pre-measured applications of an intravaginal (topical) antifungal cream or suppository. Examples are miconazole, clotrimazole, and terconazole. The medication must be inserted into the vagina even if you only have external discomfort.
Both types of treatment have relatively minor side effects.
Side effects of oral fluconazole can include:
- Nausea
- Abdominal pain
- Headache
- Rash
- Temporary changes in liver function

Oral fluconazole is contraindicated with many common medications.
However, adverse interactions of a single 150 mg dose with most of those medications are rare. Make sure your health care provider is aware of any medications that you take.
Side effects of intravaginal antifungals are usually limited to temporary burning or irritation of the affected area. Also, be aware that certain ingredients of intravaginal medication might weaken condoms or diaphragms.
“Complicated” yeast infections are those that don’t meet the criteria for uncomplicated yeast infections. Treatment for “complicated” yeast infections depends on the situation. Examples of complicated yeast infections are:
Having severe symptoms or a weakened immune system:
- Two doses of oral fluconazole taken 3 days apart is a typical recommendation. Topical treatment is not recommended.

Pregnancy:
- Pregnant people should use one of the topical creams or suppositories rather than oral fluconazole.
Recurrent infections (four or more in a year):
- Oral fluconazole is taken at consistently spaced intervals rather than only in response to symptoms. At the same time, efforts are made to identify and minimize the cause of the infection.
Symptoms are caused by an overgrowth of a species of Candida other than Candida albicans:
- Treatment depends on the species.
Treatment may be different for people with a surgically created vagina, or who are in the process of transitioning. If you have any vulvo-vaginal itching or discomfort, it is extremely important to consult your doctor for the appropriate treatment.
What About Home Remedies? There Are So Many on The Internet.
Unfortunately, there is little or no high-quality scientific evidence to show that home remedies such as garlic, tea tree oil, yogurt, or lactobacillus are effective in treating or preventing yeast infections. In fact, some of these “remedies” can be harmful. However, following a healthy diet, getting enough sleep, reducing stress, and being physically active all support immune function. Taking steps to minimize your risk factors can also be helpful.
Boric acid, widely mentioned on the internet, can be effective—but only as a professionally prescribed and dispensed intravaginal treatment for a relatively uncommon species of Candida. Do not take boric acid by mouth.
In general, the antifungal medications that are prescribed to treat uncomplicated yeast infections are effective, easy to use, relatively inexpensive, widely available, and have minimal side effects.
Do I Really Need to See My Health Care Provider for This?
We hope that you have never experienced the intense itching or the other uncomfortable symptoms of a yeast infection. But should you develop the symptoms for the first time, please visit your health care provider to ensure that you have nothing more serious.
And if, like many people, you have already had one or more yeast infections, we hope that following these suggestions will prevent another one from developing. The good news is that even complicated yeast infections are treatable. Don’t try to treat a complicated infection on your own – it’s not worth the frustration, and it is safer to let your health care provider recommend the treatment.
The convenience of being able to get over-the-counter antifungal medication in many countries has prevented a lot of suffering until a medical appointment is available. Do feel free to pop into the store to pick up a pill or a cream …but please check with your provider at least once!
How Halza Helps
Manage your health with the Halza app! Upload all test results, scans, and reports to have your complete medical history in the palm of your hand.
QuickShare your information with any attending doctor in seconds for a comprehensive diagnosis. Set health reminders to ensure you never miss a scheduled appointment or a medication dose. Share and receive words of support and encouragement on your recovery via Halza’s very own Emoji Blast!
Download the Halza app today!



