The Itch That Never Goes Away

Eczema (also known as dermatitis) is a group of conditions that cause dry, itchy, rough, and inflamed skin. Some forms of eczema are genetic, while others are due to external causes. They are not contagious but can leave affected skin vulnerable to infections such as warts and cold sores when exposed to bacteria and fungi.
Eczema flare-ups can follow a seasonal pattern and are very common during winter. So much so that it is even known as the ‘winter itch’. Dry wind when combined with indoor heating can rob the skin of moisture. For others, symptoms may worsen during summer and spring time, mostly due to sweat irritating the skin and seasonal pollen.
Most people claim that the itch is the worst part about eczema as it can be incessant. The “itch-scratch cycle” happens when itching leads to scratching, which then leads to the development of eczema and more dry skin.
Most common type of eczema – Atopic dermatitis

There are several types of eczema, that vary from mild to severe.
Atopic dermatitis (AD) is the most common inflammatory skin disease. It tends to occur during the first six months of infancy, and in young children that can last up to five years of age. Most children outgrow eczema.
Severe eczema however, follows into adulthood and is recognized as chronic eczema – long lasting with periodic flareups. Atopic dermatitis is proven to pose significant emotional burden in addition to pain, physical discomfort and sleep disturbance for millions of adults. It appears as part of a triad – rash, hay fever and asthma. This explains why individuals with a personal or family history of eczema, allergies, or asthma are more prone to atopic dermatitis.
Genes and environmental factors play a huge role in atopic dermatitis, which is primarily caused by an overreactive immune system. Some of the triggers include:
- Low humidity
- Changes in weather, humidity, or temperature
- Fragrances
- Dust mites
- Animal fur
- Pollen
- Stress
- Hormonal changes
- Immune system dysfunction
- Food allergies
How about contact dermatitis?

The second most common form of eczema is contact dermatitis. This is when a substance triggers the skin into having an allergic reaction.
Individuals who come into contact with chemicals – perhaps because of their profession – may suffer from this the most. It can also be caused by plants, cosmetics, and other allergens.
Some of the occupations typically at risk of contact dermatitis include:
Artists, carpenters, construction workers. embalmers, florists and gardeners, medical personnel, hairdressers, jewelers, painters, textile makers and veterinarians. Workplace-related eczema develops in stages, depending on the extent of exposure to allergens.
Metals and materials that commonly trigger contact dermatitis are,
- Nickel (Zippers, coins)
- Cobalt (Utensils, appliances)
- Chromium (Silverware, chrome plated jewelry)
- Deodorants and perfumes
- Skin products and cosmetics
- Harsh soaps
- Detergents
- Sweat and saliva
Unlike atopic dermatitis, contact dermatitis is solely influenced by the exposure to irritant substances, where skin cells are damaged.
What are the symptoms of eczema?

Symptoms of eczema may differ person to person.
In infants, for example, eczema affects the face, cheeks, and chin. The skin in these areas will show up more red. As they near 6 months to a year or more, it starts to affect the elbows and knees. During the crawling stage, there is a possibility of infection due to friction and bacteria growth from constant surface contact. A yellow crust, or bumps start to form on the skin. Itchy patches can also appear around the mouth, on the eyelids, behind the ears, feet, or scalp for children.
In adults, atopic dermatitis results in widespread rashes around the eyes, face and neck. Common symptoms include:
- Skin that is dry, itchy, scaly, cracked, irritated, inflamed or swollen
- Small, raised bumps that may be filled with pus
- Discoloration – Red/brown/gray-ish patches on the face or other parts of the body
- Burning sensation
- Blisters
How is eczema diagnosed?
A dermatologist or allergy specialist is best suited to access your symptoms. If there is an eczema flare up, it is good to note and share the following with them for a more accurate diagnosis:
- Medical history
- Where and where the rash has appeared
- Food and drinks consumed in the past 24 hours
- Skin products used
- Chemicals you have come into contact with
- Activities taken part in
- Home or work surroundings
Certain flare-ups are easier to diagnose; when the skin comes into contact with poison ivy for example. In situations that it is not as obvious, your skin doctor may recommend a patch test. This test evaluates factors that caused a skin reaction.

In this procedure, the skin is tested with small amounts of allergens. Patches secured with hypoallergenic tapes are attached to the skin for about 48 hours. Reactions are monitored and linked back to the allergen used. This is especially effective with individuals who may be suffering from contact dermatitis.

Skin prick testing (SPT) can also be done to find the source of allergy. Immediate reactions are accessed during a SPT, when the skin is scratched or pricked with a needle after allergens are placed, usually on the forearm.
As eczema usually starts in babies, parents can take the necessary steps by tracking family medical patterns. Is there a history of allergies? Does anyone else in the family have eczema? Such information should be shared with a dermatologist.
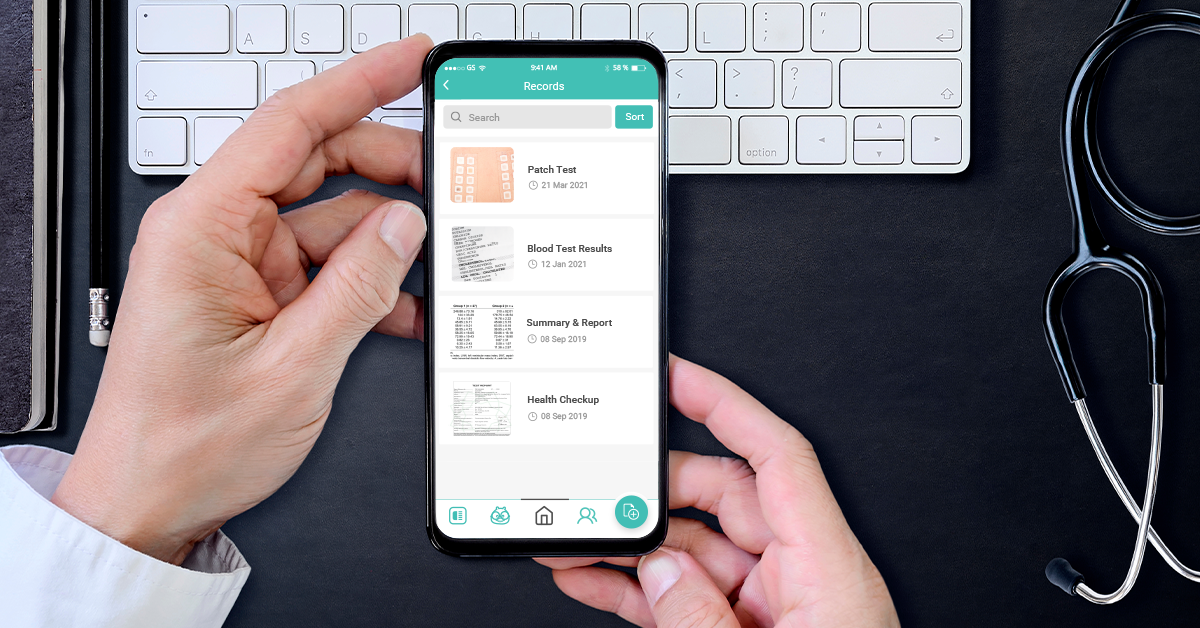
Paying attention at an earlier stage can ease and prevent the skin disorder from worsening. Halza’s Family Account allows users to manage the health of up to 6 family members.
- Store medical records
- Track allergies
- Record medication
- Monitor vital signs
Research also shows that parents who proactively tracked their child’s eczema, saw improvement in their child’s skin condition and were overall more confident in managing eczema long term.
Treating eczema
There is no cure for eczema, but the right medical/non-medical treatments, self-care measures and lifestyle changes can ease symptoms. The ideal outcome is eliminating itch as it can worsen if left untreated.
- Seek professional help
See a dermatologist or specialist, who will be able to prescribe moisturizers, topical creams, and ointments; typically used in healing the skin from the surface. Phototherapy, or ultraviolet (UV) light treatment, may be suggested for severe eczema. - Know your triggers
Once the cause of eczema is known, avoid triggers to prevent flare-ups. This can be avoiding certain fabrics and substances that irritate the skin. If eczema is caused by humidity or hot weather, individuals can be more prepared in keeping themselves cool throughout the day. - Dietary changes
Speak to a professional on possible dietary changes if food allergy is a trigger. A specialist in diet and nutrition will work with you in making changes to your usual diet.
How Halza can help?
Manage your family’s health easily with the Halza app. Store, track & share all of your child’s medical records to have them with you, wherever you go. Monitor your child’s growth and vaccination schedule as well as upload reports and doctor’s notes all with the Halza app. QuickShare a complete overview of you or your child’s health with any attending doctor in seconds, during emergencies or whenever you need.
Simplify your health journey with Halza.