Arrhythmias

A healthy heart at rest beats between 60 – 100 times a minute with an even, steady rate. An arrhythmia refers to heartbeat rates or rhythms that are too fast, too slow, or irregularly spaced.
Arrhythmias can be immediately life-threatening, moderately annoying, or nothing to worry about. They are sometimes first detected by an electrocardiogram (EKG or ECG for short) at an annual physical exam. If the result is concerning or abnormal, your health care provider might refer you to a cardiologist for further tests.
How do our hearts work?
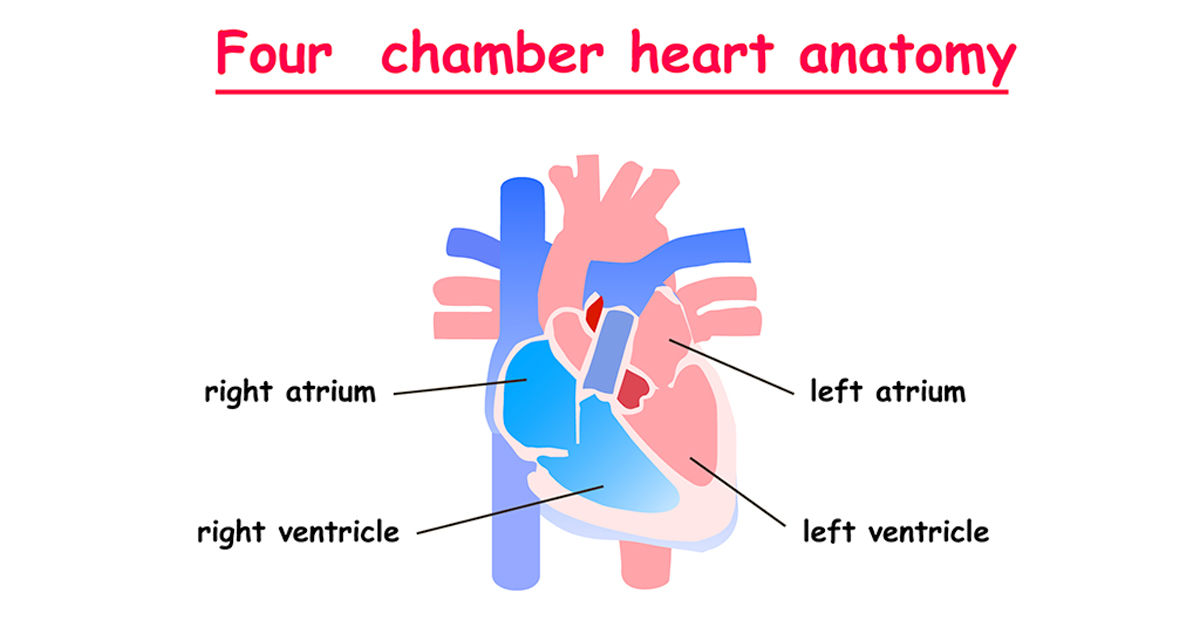
Our hearts have four chambers – a left and right atrium and beneath, a left and a right ventricle. These chambers contract in a tightly controlled rate and rhythm, enabling our blood to complete a closed loop circuit to and from the heart.
Each heartbeat should be initiated from a small area of tissue in the right atrium. called the SA (sino-atrial) node. From the SA node, the electrical signal travels through the right atrium to the AV (atrio-ventricular) node and down to the ventricles. This causes the atria to contract, followed immediately by both ventricles contracting, and then by a brief pause.
Any alteration to the heart’s electrical system will affect the rate, the rhythm and/or strength of these contractions, potentially causing an arrhythmia.
What causes arrhythmias? 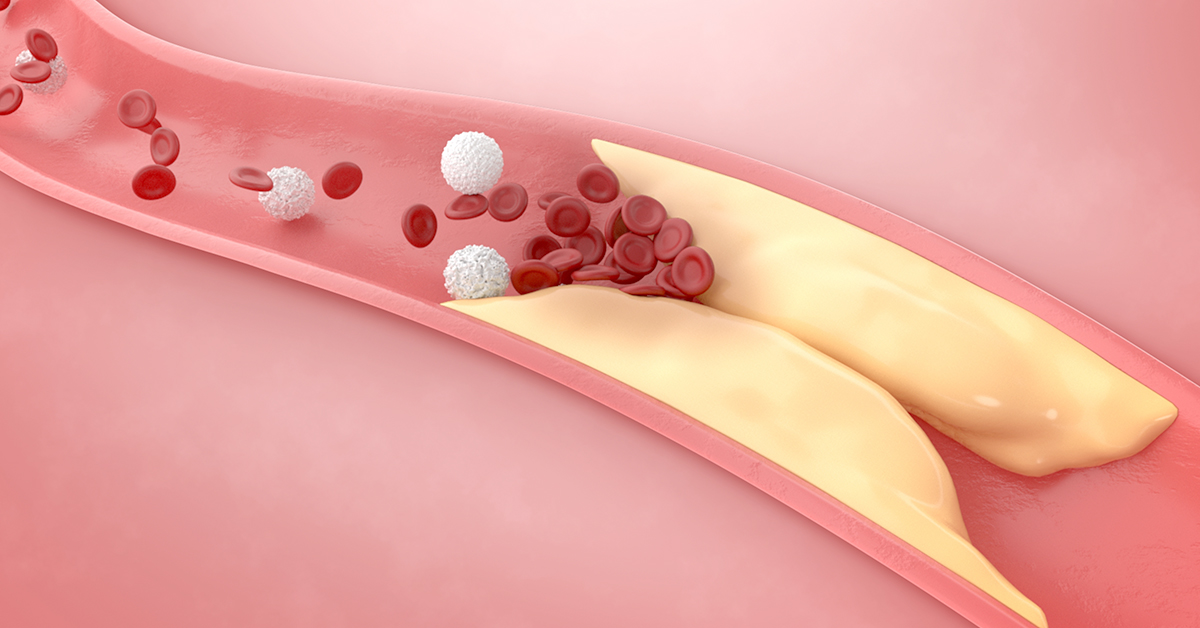
Arrhythmias can be caused by many conditions, including:
- Coronary artery disease.
- High blood pressure
- Cardiomyopathy, in which the heart muscle stretches out or thickens.
- Heart valve disease.
- Excess or deficiency of certain hormones.
- Electrolyte imbalances.
- Injury to the heart muscle. Heart attacks are a leading cause of permanent heart muscle damage.
- A genetic predisposition to heart disease.
- Conditions of the central nervous system impacting the heart’s ability to react to stimuli.
- Ingredients in some over the counter medicines.
- Incorrectly prescribed or mis-dosed prescription medications.
- Use of street drugs such as cocaine or methamphetamine.
- Sleep apnea.
- Nutritional deficiencies.
What are the most common arrhythmias?

There are many different types of arrhythmias, and many, many variations within each of those types. They can be broadly classified as sinus, ventricular, or supraventricular depending on where the electrical impulse is initiated. Sinus rhythm, in which the impulse is initiated from the SA node, is the only normal rhythm. However, a heart in sinus rhythm is considered arrhythmic if the rate of the heartbeat is too fast or two slow.

Arrhythmias most often seen by cardiologists include:
- Bradycardia:
In bradycardia, the heart beats less than 60 times per minute.
Bradycardia can be normal, such as during sleep, or in athletes with very strong hearts. It becomes dangerous if the heart continues pumping too slowly to effectively circulate blood throughout the body, or if the heart rhythm is irregular.
- Tachycardia:
In tachycardia, the heart beats more than 100 times per minute.
The chambers contract too rapidly to fill up with the normal amount of blood, and less blood gets pumped to the rest of the body. This leaves our organs and tissues short of oxygen and necessary chemicals and nutrients, and without a way to remove waste such as carbon dioxide.

However, as with bradycardia, tachycardia is not always dangerous. For example, when we exercise, we intentionally raise our heart rate, thereby strengthening the muscle. Our heart rate might rise before a medical appointment, or if we witness something scary. Those are transient events with a regular rhythm arising from the SA node.
- Ventricular tachycardia (“V-tach”):
V-tach is a rapid heart rate in which the electrical impulses originate from the ventricles instead of the SA node. This is a life-threatening emergency that can lead to ventricular fibrillation (“V-fib”) or to cardiac arrest.

- Ventricular fibrillation (V-fib):
V-fib is caused by numerous disorganized, rapidly firing electrical impulses. The ventricles quiver instead of contracting productively. If treatment is not started immediately, the heart will stop beating. The defibrillators that you may have seen in schools, airports, or other public places are there to treat this emergency condition.
- Premature ventricular contractions (PVCs):
A PVC is an extra beat that is initiated in one of the ventricles. PVCs might feel like a skipped heartbeat or a slight fluttering.
In the healthy heart, occasional PVCs are not necessarily worrisome. They might be caused by caffeine or too much stress. However, PVCs can also be caused by electrolyte imbalances, anemia, thyroid disease, heart disease or numerous other conditions that shouldn’t be left untreated.
- Atrial flutter:
Atrial flutter is a rapid heartbeat that originates in the atria. After the initial firing from the SA node, the electrical signals move throughout the atrium, causing it to contract faster than the ventricle below.

- Atrial fibrillation (“A-fib”):
A-fib is a condition in which the atria contract rapidly and irregularly, resulting in diminished force of the contraction. The atria don’t actually need a huge amount of force to push blood down into the ventricles, yet A-fib is an extremely serious condition. Since blood isn’t effectively forced out of the atrium into the ventricle, some of the blood settles in the atrium. Over time, there is a good chance that the pooled blood will form a clot. If this clot is in the left atrium and it breaks away, it will travel to the left ventricle. From there, it will be pumped out of the heart, usually to the brain where it will cause a stroke. Strokes caused by A-fib tend to be severe and result in significant and permanent loss of function.
- Heart block:
A heart block results from a defect in the normal electrical pathway. This delays or prevents the electrical impulse from traveling from the SA node to the ventricles. Heart blocks range from mild to severe.
- Long Q-T syndrome/Torsade de pointes:
Long Q-T syndrome is a condition in which the heart’s electrical system takes too long to recharge between beats, leading to tachycardiac arrhythmias. Torsade de pointes is the term for the arrhythmia most associated with Long Q-T syndrome.
What are the symptoms of arrhythmias?
Some arrhythmias don’t cause any symptoms and are only discovered during a routine check-up. Others cause symptoms including:
- The sensation that your heart missed a beat.
- Heart pounding.
- Dizziness.
- Lightheadedness.
- Shortness of breath.
- Chest discomfort.
- Fatigue.
- High fever.
How are arrhythmias treated?

Treatment for arrhythmias first depends upon what type of arrhythmia the person has. Some other considerations include age, co-occurring medical conditions, availability of medical expertise and resources in the patient’s location, and sometimes finances. Treatments include:
- Lifestyle changes such as improving diet, exercising, reducing stress, treating sleep apnea, and stopping smoking.
- Medication.
- Pacemakers.
- Biventricular pacemakers and defibrillators, also known as cardiac resynchronization therapy.
- Cardiac catheterization.
- Catheter ablation. Uses high frequency energy to destroy the tissue that is causing the arrhythmia.
- Surgery.
- Cardioversion. This is done in a medical facility under anesthesia. An electrical impulse is delivered to the heart which starts a normal rhythm.
- Implantable cardioverter-defibrillators.
- Pulmonary vein isolation: Creates scar tissue around the area that is initiating A-fib.

Covid-19 has been a significant cause of new-onset cardiac arrhythmias, which can last long after recovery from the virus itself. Arrhythmias may be responsible for some symptoms of what has become commonly known as “long Covid”. People who have underlying heart disease at the time they develop symptoms of Covid-19 are more likely to develop an arrhythmia; however, long-lasting arrythmias can and do develop in people with initially healthy hearts. The more severe the symptoms of Covid-19, and the more intensive the treatment, the higher the likelihood of developing a long-lasting arrhythmia. In addition to the risk posed by systemic shock, widespread inflammation, and low levels of oxygen, particular correlations have been noted in some hospitals between the use of certain lifesaving medications and the subsequent development of Long Q-T syndrome, and between the use of mechanical ventilation and development of atrial fibrillation.